Hypothesis: An aetiological model of chronic pain and CRPS : Phases of the same inflammatory condition
This page will follow the whole article with the same name with many explanations. An officially published article needs shortness. ,In this case it requires a broad professional knowledge of different medical specialisms too. This kind of knowledge is apparent very seldom. Super-specialists don't have sufficient insight in the knowledge of other super-specialists. And that's the real problem of chronic pain. It is clear that the explanation of the origin of chronic pain cannot be short. This page will be added as a Blog adjusted with new content and adapted to questions received.
1 March 2018 Posting 1.
What does the title mean?
This paper shows a new model about the origin of chronic pain and CRPS (Complex Regional Pain Syndrome)
What's already known about chronic pain:
- 1886: Head: chronic pain areas are localized in the SKIN, produced by viscero-cutaneous reflexes.
- 1954: Baumann and Ueckert : 70% of chronic pain areas in the skin are Cold. (measuring with electrical galvanometric equipment on the skin)
- 1960-1980: introduction of non-contactile infrared thermography : skin surface temperature measuring by means of infrared irradiation.
- 1969: synthetic production of prostaglandins
- 1977: Horrobin and Manku published dosis-effect curves of prostaglandins
- 1969-1980: Many publications about prostaglandin effects: relation with pain, inflammation, nervous action and immunology.
- 1982 : van der Veen: viscero-cutaneous reflexes exist in human beings
- 1982: van der veen: 75% of chronic pain areas in the skin are Cold
- 1989: van der veen: 70% of chronic pain areas improved by PTX : temperature changes in the skin area.
- 2008: Arendt-Nielsen e.a.: Pain area originated in the gut is reflected by viscero-cuteous reflexes and can be found with infrared thermography in the skin.
It is obvious that there are five elements (influencing each other) you have to consider in the investigation of chronic pain:
- Skin
- Skin temperature
- Infrared Thermography
- Viscero-cutaneous reflexes
- Prostaglandins
which have a related interaction with each other.
Next post: What's a Head zone and what is the relation with skin temperature and pain?
Henk van der Veen 01-03-2018
3 March 2018 Posting 2.
What's a Head zone and what is the relation with skin temperature and pain?
In 1898 the medical scientist: H.Head discovered pain sites on the skin. Those sites has been named by his name; they are called Head’s areas. Although tree years earlier the German homeopath Weihe found 195 continuously recurring pain sites in the skin by different diseases his name is not attached to this discovery.
The Head’s zones or Head’s areas has been described extensively in a German study book edited in 1962. (Hansen und Schliack: “Segmentale Innervation, Ihre Bedeutung für Klinik und Praxis”). 1962 wasn’t a good timing. After the second world war the supremacy of the German medical science had been collapsed. Scientists had been divided between the US and the USSR. The official language in Western universities had been changed to English. So nobody could learn from the early ideas about chronic pain. Curious is the fact, that four publications of H.Head are published in the English language and only one in German:
✓ “On disturbances of sensation with especial reference to the pain of visceral disease” . Brain. London 16 (1893),1-133 and 17 (1894),339.
✓ Die Sensibilitätsstorungen der Haut bei Visceralerkrankungen. Hirschwald Verlag Berlin 1898
✓ with AW Campbell: The pathology of herpes Zoster and its bearing on sensory localisation. Brain. London 23 (1900),353,523
✓ with WHR Rivers: The afferent nervous system from a new aspect. Brain London 28 (1905) 99-115
✓ A human experiment in nerve division Brain 31 (1908), 323
Herpes zoster is a viral infection, which transports itself along the nerve fibers and ends in the skin. The research of Head shows a segmentally built nervous system and skin system too.
That skin system is called dermatomes. You can regard this in modern times as a stack of computerised units intensively related to each other. Each unit is called a segment. In embryological stage human beings are built from such segments:
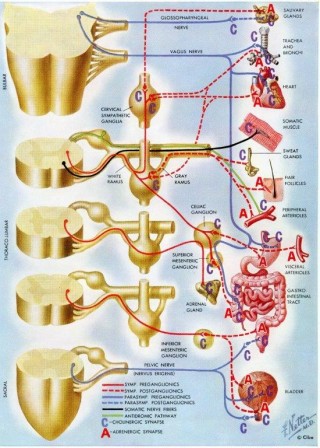 Above you can see the central nervous system, built up from segments. Picture from Frank G Netter: Ciba Collection. Nervous system 1967.
Each level has been connected with specific areas in the skin, muscles, skeleton, vessels and organs.
H. Head showed the relationship of pain between organs and their specific areas of the skin in 1898 already. In living human beings however the existence of those relationships has been showed by Van der Veen (1982, published in 2012) and Arendt-Nielsen and his group (2008). Arendt-Nielsen has demonstrated that pain, generated in an organ generates pain in a related area in the skin as well.
The skin is also divided in segments (dermatomes):
Above you can see the central nervous system, built up from segments. Picture from Frank G Netter: Ciba Collection. Nervous system 1967.
Each level has been connected with specific areas in the skin, muscles, skeleton, vessels and organs.
H. Head showed the relationship of pain between organs and their specific areas of the skin in 1898 already. In living human beings however the existence of those relationships has been showed by Van der Veen (1982, published in 2012) and Arendt-Nielsen and his group (2008). Arendt-Nielsen has demonstrated that pain, generated in an organ generates pain in a related area in the skin as well.
The skin is also divided in segments (dermatomes):
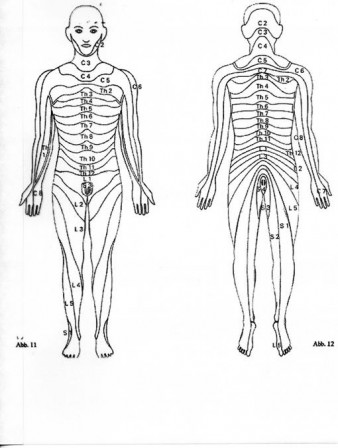 In case of pain generation the temperature of that specific skin area changes. Infrared thermography can measure these changes.
In case of pain generation the temperature of that specific skin area changes. Infrared thermography can measure these changes.
!!!Next post: the temperature of Head’s zones.
Henk van der Veen 03-03-2018
7 March 2018 Posting 3.
SKIN temperature: the temperature of the HEAD's zones.
The temperature of Head’s zones
In 1954 Baumann and Ueckert published the results of a study about the temperature in Head’s zones. In 70% of the cases the temperature was lower in relationship to the surrounding area. The possible conclusion could be: in painful zones the skin temperature is lower in 70% of the patients. 25 years later new opportunities in temperature measuring (infrared thermography) could check these results. (van der veen: 1989, published in 2014).
The results of Baumann and Ueckert could be verified.
That leads to the first question: WHY does this happen and a second question: HOW ?
What can we conclude at that moment ?
First: In case of chronic pain there is something that happens IN THE SKIN. As a result in most cases the SKIN temperature is reduced.
Secondly: infrared thermography gives you the opportunity to observe and measure contactless in a objective way.
You have to realise that the measurements are observable by anybody who is interested.
Perhaps that’s the reason, that the origin of chronic pain has been hidden for more than a century !
Head had stated, that processes in the internal organs could give a reaction in all of the segmental related structures, so also in the SKIN. It means, that reversely a change in the skin
(for example the temperature of the skin) has a change in temperature in the internal organs.
In 1925 the Danish researcher Wernøe showed with experiments in Elvers that irritation of the skin resulted in vasodilation in internal organs. This kind of reaction is called: a Cutaneous-visceral reflex. The reversed way from internal organ to skin is called: a visceral-cutaneous reflex. (Head).
But it has lasted to 1982 before this kind of reflex could be demonstrated in living humans.
(van der veen 1982, published in 2012 and Arendt-Nielsen and his group in 2008)
From this time we know, that stimulation of an internal organ results in an increase in temperature in a specific predictable area of the skin.
We can see and measure that with contactless infrared thermography.
Conclusion: if there is a skin area with chronic pain we have to measure the temperature of this area and the surrounding skin areas.
What can we deduce from this:
Head proposed a relation between internal organs and painful zones in the skin. That relation is confirmed now: a painful zone in the skin of a living human being can have a temperature change too. Besides this the temperature of the skin in chronic pain is mostly lowered (70%), sometimes raised (20%). Visualisation is possible with contactless infrared thermography.
An example from 1981. After an appendicitis operation: Phantom pain: fig.3.
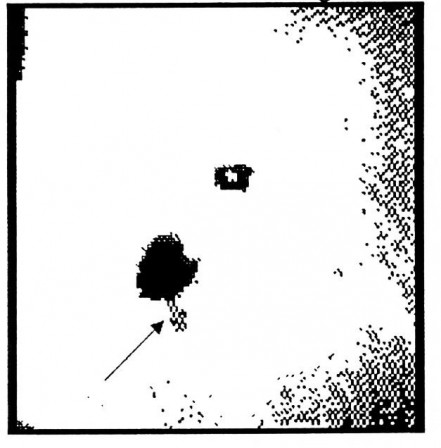 1980: You see the navel as a square in the middle. The operation area is very cold (black spot). The arrow points to the so called “point of Mc.Burney”. The most painful place in the painful area. Clearly a phantom pain, representing a cold area in the skin. Local anaesthetic of this skin area gives as a result disappearing of the pain for some hours immediately after injection.
The same picture projected on a body figure: fig.4.
1980: You see the navel as a square in the middle. The operation area is very cold (black spot). The arrow points to the so called “point of Mc.Burney”. The most painful place in the painful area. Clearly a phantom pain, representing a cold area in the skin. Local anaesthetic of this skin area gives as a result disappearing of the pain for some hours immediately after injection.
The same picture projected on a body figure: fig.4.
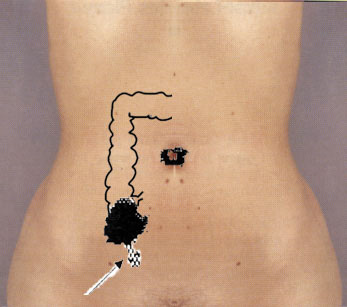 From casuistic we know that using an anaesthetic in the point of Mc Burney in case of an acute appendicitis lets disappear the sharp pain, but leaves the existing dull, nauseous pain. You can use that if you need a diagnosis. So the same cause (Inflammation) in the internal organ gives raise to two kinds of pain: one from the viscera it self and one transferred from the viscera to the skin by a visceral-cutaneous reflex. But after an operation you can see a second effect: chronic pain, released in the skin in a situation of phantom pain. In this case the most painful place is NOT the operation scar, but the skin itself.
Another example:
Fig.5.
From casuistic we know that using an anaesthetic in the point of Mc Burney in case of an acute appendicitis lets disappear the sharp pain, but leaves the existing dull, nauseous pain. You can use that if you need a diagnosis. So the same cause (Inflammation) in the internal organ gives raise to two kinds of pain: one from the viscera it self and one transferred from the viscera to the skin by a visceral-cutaneous reflex. But after an operation you can see a second effect: chronic pain, released in the skin in a situation of phantom pain. In this case the most painful place is NOT the operation scar, but the skin itself.
Another example:
Fig.5.
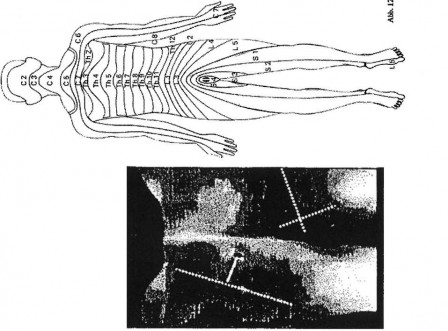
Fig.5. 1981: A man, lying as the schematic person. The buttocks (pointed) are black (cold). Scars from a dog attack from behind three years before. The dotted lines represent the perimeter of the wound: Result: Chronic pain.
Fig.6. 1982
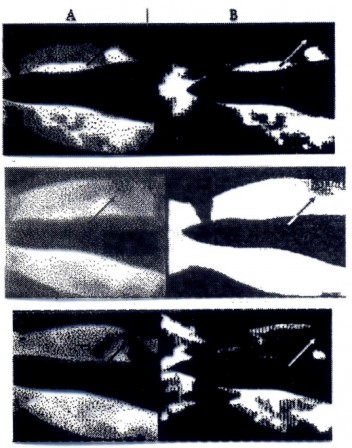
Fig.6. An owner of a flower shop fell over a bucket and got a proximal radius fracture on the left arm (See arrow). He received orthopaedic treatment that was completed, technically with good results. Severe pain persisted that became intolerable after a few hours when lifting. It disappeared after a relaxed weekend, but returned after slight exertion. Clinical defects were no longer found. Infrared thermography images were made in 1980 (shown under Column A). The original thermography images, recorded with photographic film in those days, are under Column A. A hanging camera with a mirror was also used with this patient, hence the patient's left side is on the right (Notice the wristwatch in Column B). There was severe asymmetry to the disadvantage of the left after exertion. Black represents less blood circulation here too. After rest (the most central under Column A) is almost symmetrical. After slight exertion (Column A in the lower photo) also shows massive asymmetry. Column B is technically filtered on threshold value. Everything under the threshold value is black. Everything above is white. It clearly shows the differences. A blood circulation dip can be seen in the area of the fracture even at rest.
So you can see the chronic pain areas with the help of infrared thermography. That is the only way to get chronic pain visible and measurable. In this examples you can see temperature changes by traumas in the skin, but also by visceral- cutaneous reflexes from internal organs. The impact of Head’s research. What did we learn about chronic pain in this stage?: Chronic pain is settled in the skin, can be produced by traumata from the skin and underlying tissue, but also as a result from (old) processes in de internal organs as a part of the complexity of all the segmental areas via visceral-cutaneous reflexes. The WHY and HOW of the “WHY this happens and a second question: HOW? of the Head’s zones” is answered now.
Next post about contactless infrared thermography.
Henk van der Veen, 07-03-2018.
14 March 2018 Posting 4
Contactless infrared thermography.
The method of Baumann and Ueckert to measure the skin temperature has been succeeded in the sixties by measurement with contact crystal plates and much better (and more expensive) contactless infrared thermography. It should not to be mixed up with infrared photography. Thermography is a computerized technique in which the images have been built up and stored with the values of the frequency of the measured infrared light spectrum. (Wikipedia: https://en.wikipedia.org/wiki/Thermography : “infrared thermography”: Thermographic cameras usually detect radiation in the long-infrared range of the electromagnetic spectrum (roughly 9,000–14,000 nanometers or 9–14 µm) and produce images of that radiation, called thermograms.) For medical purposes the equipment is appropriate in measuring the skin temperature. De light frequency of the emitted infrared radiation of the skin has been computed to temperature values. In the eighties every huge factory in electronics had a concept of a thermograph for breast cancer screening. For researching of the chronic pain field we have used a Philips thermograph from 1980 till 1995.
fig.7.

You could make pictures like these:
Fig.8.
Vertically on the right side of this polaroid picture from 1980 there is a temperature bar :10 degrees Celsius divided in artificially colours of one degree each. Yellow and white being the highest temperatures and blue and black the lowest. One can see here a great temperature difference between de right and the left arm. The dark green is the painful one. Another sample:
Fig.9.

A picture of the back. You can see here isotherms: an isotherm is a curve with the same value in temperature. All the points combine points of equal value. The red one in this sample has a temperature of 33.3 degree Celsius. The blue one has a difference of 0.3 degree Celsius : 33.0 degree Celsius. This picture is a very interesting sample of a computed infrared image. A third sample from 1978: Philips demo with the same temperature range as the sample one.
Fig.10
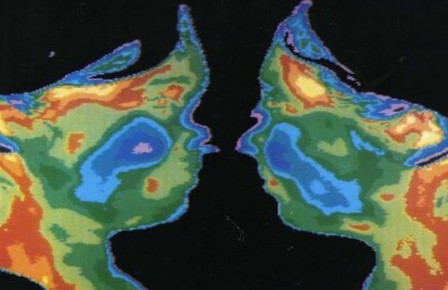
The equipment was voluminous and difficult to manage. The infrared sensor had to be cooled with liquid nitrogen. In 2018 there is a new generation of thermographic cameras. Everything in one. Measuring by software on a normal computer.
Fig.11.
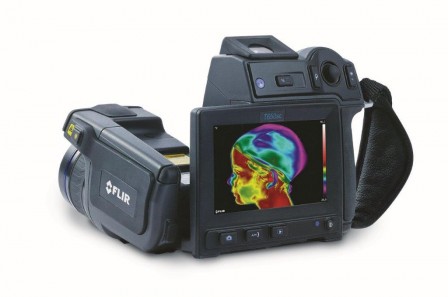
But what we are measuring is the same as in 1980. Painful sites. In experiments in 1982 and 1989 we had found (and published that in 2012 and 2013) the same results as Bauman and Ueckert: about 70% of the painful places are so called cold spots, they are lower in temperature, 20% are hot spots, they have a higher temperature. That’s very interesting. You can find something, objectively on painful sites and make it visible, while the regular Medicine is thinking: maybe there was some problem in the past, but the signal has lost its function in the present. Therefore many psychologists and psychiatrists have a job in treating chronic pain. This discrepancy in temperature in painful sites started the investigation to the origin of chronic pain. Investigation with infrared thermography. This research leads to new questions. We found several conflicting data:
Next in Post 5.
The discrepancies in thermographically dates
Henk van der Veen, 14-03-2018
27 March 2018 Posting 5
The discrepancies in thermographically data.
Since the Greek and Roman times inflammation has been associated with swelling, redness, pain and warmth. Would it be possible that there are inflammations without these characteristics? That has to be investigated by the relatively new method of Infrared thermography. Next to this method you can investigate the same symptoms with Technetium scanning and with a biochemical method with blister fluids. Technetium is a radio-active material with a short tissue half-time, but still it gives radiation. The method is neither cheap nor simple. Blister fluids taken off from pain sites is not an agreeable process for the patient. It isn’t cheap and simple. Infrared thermography on the other hand measures the warmth of the body-skin . It is easy, doesn’t incriminate the integrity of the human body and relatively cheap. Therefore it should be the first choice in case of pain investigation. But we found interesting discrepancies in this kind of research.
- why are painful sites 70% cold and in 20% warm. What is the meaning of this finding?
- why is it possible to see painful sites on the skin?
- what is this meaning of this in case of differential diagnosis in Medicine ?
- why causes “cold stress” or “Cold strain” in some persons temperature decreasing on pain sites and in others temperature raising?
- why causes stimulation of the autonomic nervous system the same effects on skin temperature as cold stress ?
- Why does CRPS (Autonomic reflex dystrophy) in the end phase appear being a cold site with inflammatory active proteins like the cytokines Interleucine-1 and Interleucine-6 ?
All described above seems to be very confusing. Is infrared thermography the promising method, that had been expected or is it rubbish? It is confusing like the research about prostaglandins: many results are conflicting with each other. More: they are mutual negations. There is a relation between vasoactive events and prostaglandins. There is a relation between vasoactive processes and infrared thermography too. So there has to be a relation between infrared thermography and prostaglandins. An analysis of the mentioned contradictions has been described for the field of prostaglandins in 1977 already. An analysis, completely forgotten in 2018. If that analysis is applied to thermographically results, the results are not contradictions any more.
What we can learn in these five postings? Pain research has a long history. The publications were mainly written in the German and French language. After the second world war scientists have been evacuated from Germany to the united Kingdom, United States en USSR. After that only a few scientists could read in German and French scientifically literature afterwards. New publications had been appeared in English. Therefore the knowledge about the origin of chronic pain has been mostly disappeared . However without this knowledge chronic pain as a biological process cannot be understood completely. Modern insights about temperature changes of the skin and related organs is leading to possibilities in visibility and measurability of chronic pain sites. The what and why has been enclosed in old German research. Contactless infrared thermography had been going in. However the link for understanding the whole process was missing. That changed with the introduction of Prostaglandins.
Next Post: prostaglandins
Henk van der Veen 27-03-2018
18 April 2018 Posting 6.
Prostaglandins
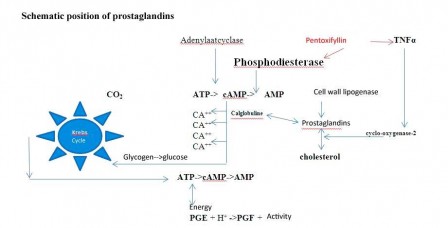
Prostaglandins are substances that are produced in several locations throughout the body and that have hormone-like effects. Hormones, however, are formed in specific organs and then released into the blood stream. They regulate metabolic processes of distant (sometimes very distant) other organs. The actions of prostaglandins resemble the actions of hormones, but prostaglandins are produced at the site of their action. Also, they are broken down at these sites very rapidly. Within minutes! They are derived from cholesterol or during the breakdown of cell membranes.
 Prostaglandins are very special substances.
Prostaglandins are very special substances.
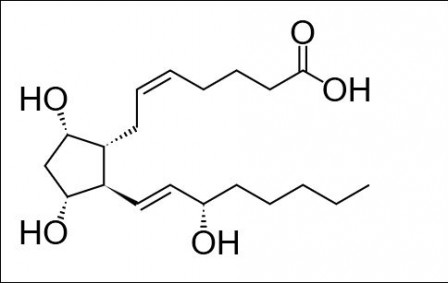 Prostaglandin F2 alpha
Prostaglandin F2 alpha
They do not have a biological effect by themselves. They bind to endogenous molecules or to drugs, which do not have an effect by themselves either. In combination, like a jockey and a horse, they show biochemical activity. There is no life without prostaglandins. The amount of prostaglandins determines the nature of the action of his buddy. For example: noradrenaline is a vasoconstrictor when bound to a low concentration of a matching prostaglandin, but when bound to a high concentration, it has a vasodilator effect. There are many examples like this. Prostaglandins act on a wide variety of processes. For this website, the effect of prostaglandins on inflammation and pain is of particular interest. Prostaglandins bind to inflammatory proteins and activate or inhibit them. Inflammations are characterised by three classical signs: swelling, redness and pain.
 CRPS
CRPS
Swelling is caused by leakage of fluids from the blood vessels, redness by vasodilation and pain by the stimulation of the nerves running through the inflamed site. Prostaglandins play a role in the development of the three signs.
Since prostaglandins are broken down so quickly, it is difficult to subject them to biochemical research. If you take them from a tissue, you need to study them very quickly before they are broken down. An even more difficult problem is that prostaglandins are biologically active at very low concentrations: a millionth of a billionth gram per millilitre: 10-15. Every disturbance of a tissue easily causes the release of a million times more prostaglandins.
This problem seemed to be solved when, in 1969, it became possible to synthesise chemically stable prostaglandins. Thousands of articles were published about the action of administered prostaglandins. Unfortunately, the results of the studies were often contradictory. Noradrenaline, for instance, was found to have a vasoconstrictor effect by some researchers and a vasodilator effect by others.
In 1977, two pharmacologists from Nova Scotia (Horrobin and Manku) conducted a very special study with muscle-vessel preparations. They first stopped their own production of prostaglandins in the tissue and tested it with noradrenaline. Nothing happened. Subsequently, they added tiny amounts of prostaglandins: from picograms (10-12 gram per millilitre) to more than 100 nanogram (10-7 gram per millilitre). So this ranged from a millionth of a millionth gram per millilitre to a tenth of a millionth). This produced clearly measurable results.
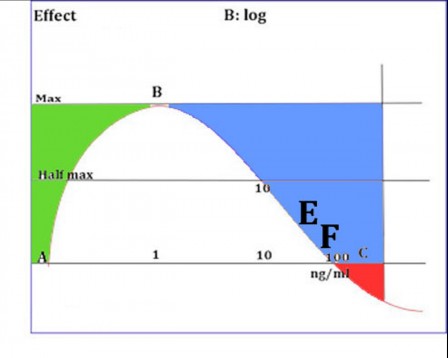
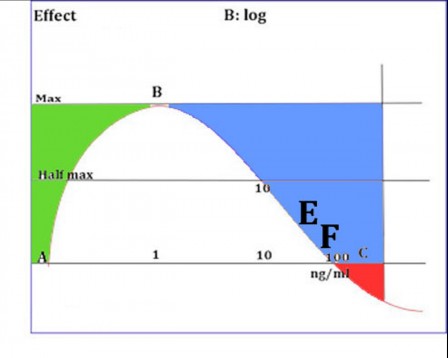
The researchers plotted the results in a graph, with the amount of prostaglandins on the horizontal axis and the contraction force of the muscle preparation on the vertical axis. When the contraction increased, the flow rate through the vessel decreased. Maximum vasoconstriction was reached at 1 nanogram prostaglandins per millilitre.
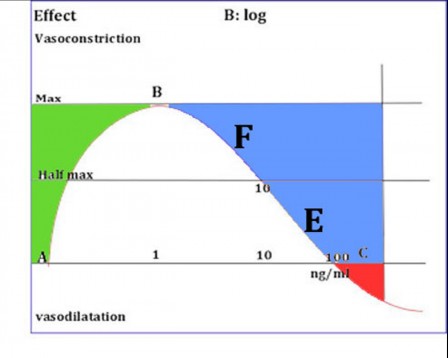
Fig.1 B
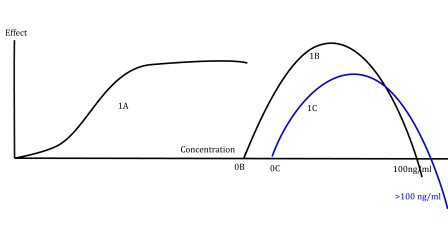
When they administered more prostaglandins, the constriction decreased and the flow rate increased again. With 10 nanogram, they found only half the maximum vasoconstrictor effect and with 100 nanogram the effect was zero. When they administered more than 100 nanogram, the flow rate INCREASED due to VASODILATION. So the effect reversed. The resulting curve is called a bell curve.
What is the significance of these findings? The prostaglandin they studied acts as a light switch: light on or off. In this example: vasodilation or vasoconstriction. It is even a dimmer switch: more or less power makes the light stronger or weaker. In this example: larger or smaller amounts of prostaglandins increase or reduce the diameter of the blood vessels. As a result, the flow rate also increases or decreases. In the body, a higher flow rate means a greater heat supply. Like with floor heating, a larger supply of heat means a warmer floor. The floor is comparable to the human skin and the temperature of the skin can be measured, just like that of a floor, by means of a special infrared or thermographic camera. The regulation of skin temperature is discussed in Postings 1,2 and 3, the infrared camera in Posting 4, the apparent contradictions of the infrared measurements in Posting 5. However, as described above, the contradictions are not all that contradictory. It can simply depend on the prostaglandin concentration in the measured site of the skin and the internal organ corresponding with this site.
The first paragraph of this Posting already mentioned the link between prostaglandins and pro-inflammatory proteins or cytokines. Two types of prostaglandins play an important role in CRPS and chronic pain: the vasoconstrictor and vasodilator prostaglandins PGF and PGE. But let’s not make the model too complex, so that non-experts will also be able to understand this.
Imagine that a vasoconstrictor prostaglandin (PGE) binds to a pro-inflammatory protein. As long as the PGE concentration is smaller than 1 nanogram per millilitre (ng/mL), the vasoconstrictive effect increases. The blood vessels contract, creating a feeling of cold. Similar to the sensation at the beginning of a flu infection. If the PGE concentration increases, the vasoconstriction will decrease. The temperature rises and the inflammation becomes noticeable. The amount of cytokines also increases. As soon as the PGE concentration increases to more than 100 ng/mL, the blood vessels dilate. The cytokines are supported maximally by the prostaglandins and the inflammation strikes: the patient has the flu. During the recovery, the PGE concentration drops again. The cytokine concentration also decreases. The temperature goes down. When the PGE concentration falls below 100ng/mL, the prostaglandins resume their vasoconstrictive action. The temperature now drops very quickly. The closer the PGE concentration reaches 1 ng/ml, the more the blood vessels contract and the temperature (of the skin) decreases. If the inflammation is not a general disease - such as the flu - but a local inflammation, a cold spot can be identified by means of infrared thermography. The spot is cold compared to its surrounding and will contain pro-inflammatory cytokines. Their presence means the patient has a chronic inflammation.
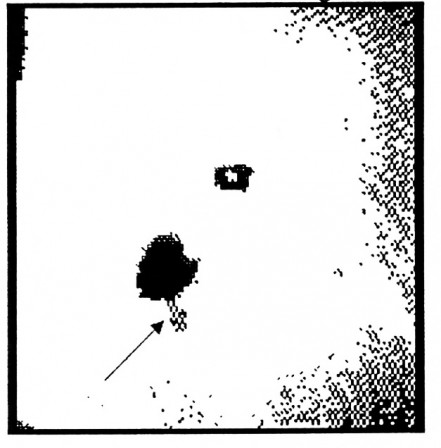 __Belly scar after excision of the appendix. Phantom pain. Follow the pointer.
Photography with infrared technics.1980.__
__Belly scar after excision of the appendix. Phantom pain. Follow the pointer.
Photography with infrared technics.1980.__
Projected on the body:
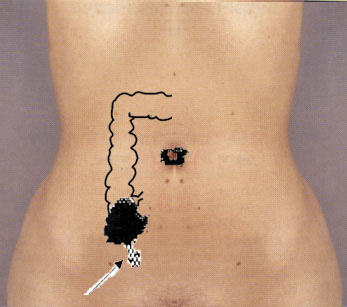
Chronic pain: a result of COLD chronic inflammation.
However, inflammations that do not present with the classical signs of redness and swelling are usually not diagnosed as inflammations. This has been scientifically proven for CRPS (complex regional pain syndrome), previously known as reflex sympathetic dystrophy syndrome. A PhD thesis has been written about this. This has not yet been demonstrated to apply to chronic pain as well, simply because no one was interested in studying it. But chronic pain apparently always develops after an inflammatory event: a local inflammation, fracture, haemorrhage, injury or wound. These events are always accompanied by the formation of pro-inflammatory cytokines and prostaglandins always play a role in it. There is no reason to assume that there would not be any cytokines left behind during recovery, like in the case of CRPS. This proves that a chronic inflammation, caused by cytokines and prostaglandins that are left behind, is the most likely explanation for the development and maintenance of chronic pain.
18-04-2018 Henk van der Veen.
Next posting: Present: The consequences of the findings from the past.
22 April 2018 Posting 7.
Present: The consequences of the findings from the past.
In six postings we have seen the effects of the nervous system, especially the autonomous part of it. Diseases in the hidden areas of the body are detectable in and on the skin, manually and visually by well-educated doctors and moreover by technically assisted computerized infrared thermography.
The way this is happening is called “Visceral-cutaneous reflex”, a loop of the central nervous system.
But that is not the whole story. There is something between the internal process , the nervous system and the skin. Something, that’s triggering the activity of all of these intermediates: biochemicals, called “Prostaglandins”. These biologically active molecules are showing regulatory and modulating activities. They are activating inflammations, regulating the blood flow in the vessels, activating nerve activity and producing pain. That’s the reason, why doctors are giving prescriptions for painkillers. These drugs (like aspirin, diclofenac, indomethacin, also called "NSAID") are diminishing the production of prostaglandins!
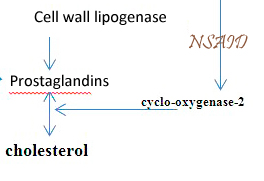
Above you see the production way of prostaglandins. One way from the cell wall, stimulated by the cell wall lipogenase. Another way from cholesterol, stimulated by cyclo-oxygenase-2. This enzyme is blocked by NSAID.
Prostaglandins do have another speciality: They can function as a switch, which can invert the activity of human biochemicals to the contrary. Impairment or improvement of the blood flow for example.
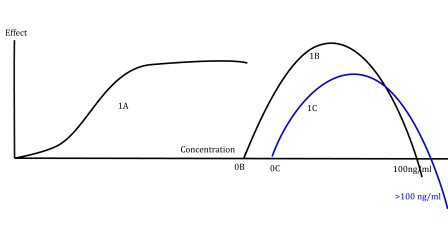 Fig.1A is a "plateau-phased"curve; Fig.1B is a "Bell-phased"curve; 1C is a combination of both.
Fig.1A is a "plateau-phased"curve; Fig.1B is a "Bell-phased"curve; 1C is a combination of both.
You see the switch moment at 100 ng/ml beyond point "B"
Just dependent on the concentration. We don’t know any other system in the human body with the same property. Without these prostaglandins: no pain, no inflammation, no visceral reflexes, no infrared thermography, no life. You can image it for yourself as a locally fire after a bone fracture, an infection, a wound, a haematoma. Such a fire is a very complexly process. It needs energy and biochemicals for modulating and regulating actions. These biochemicals are produced locally, partially computer-controlled by the autonomic nervous system and partially by the produced biochemicals itself. These biochemicals like prostaglandins and cytokines are stimulating nerve ends. This stimulation is transported along the nerve fibres to the pain centre in the brain. For pain experience two types of fibres exist : thin fibres without isolation and thick fibres with isolation. Thin fibres are responsible for burning sensation. Thick fibres for normal pain sensation. In some situations the local fire can damage the isolation layer of the thick fibres. (Like electrical wires: without isolation and with isolation) See: http://pediaa.com/difference-between-myelinated-and-unmyelinated-nerve-fibers/
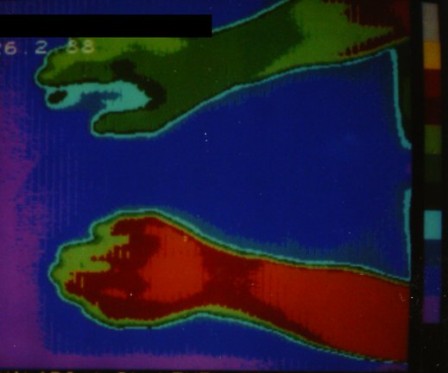
The result is changing thick fibres into thin fibres and a burning sensation by stimulation through prostaglandins and cytokines. This sensation can be diminished or even released by prostaglandins blocking agents like aspirin and by cytokines blocking agents like Pentoxifylline (PTX) or (modern) Infliximab. They are blocking agents of TNF-alpha both. The price of Infliximab is about 100 x the price of pentoxifylline. Curious is the fact, that chronic pain has two forms of representation: infrared thermographically COLD or WARM. A Cold spot is in a vasoconstrictive state always. A hot spot always is vasodilatative. Both of them can be present in the same patient in the same moment. Curious is the fact too, that PTX upgrades the Cold spot to a normal value and in the same time the Hot spot downgrades to normal value.
Two contrarily effects on the skin blood flow in the same time from one medicine. And moreover: the pain is diminishing in both areas.
There is a possible explanation for this: from PTX two types of action have been known at least: at first blocking of the enzyme phosphodiesterase. Result: better perfusion of the vessels. Cold spots are upgrading in temperature.

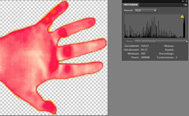
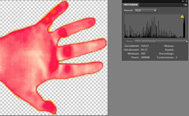
This example shows the change after PTX medication. Before and after. The hands (warm) have been downgraded in temperature. The arms have been upgraded. Patient with crps onset left hand
But this doesn’t give an explanation for the temperature downgrading in hot spots.
Explanation two:
If we have a look at CRPS, we know that the hot spot is representing an inflammation.
We have seen, that an inflammation has three characteristics: redness, swelling and pain.
 An inflammation is produced by the combined action of prostaglandins and cytokines.
If we are blocking the action of cytokines, we are blocking the inflammation too.
Infliximab is such a blocking agent. Two patients with CRPS had been cured by that.
The skin temperature is downgraded to normal as well.
In the hot spots of chronic pain the pain and the skin temperature has been downgraded by PTX. PTX and Infliximab have a -scientifically demonstrated- commonly effect: blocking of the inflammation activating cytokine: TNF-alpha. TNF-alpha actvivates the production of prostaglandins from cholesterol.
If the effect of PTX into painfully areas has been caused by the TNF-alpha blocking property the painful warm area in chronic pain must be caused by an chronic low profile inflammation! For this exists another scientifically argument.
In the end situation of CRPS the skin temperature is downgraded beneath the normal temperature. However pain exists as yet. One is seeing the same situation in case of cold chronic pain. In CRPS has been scientifically demonstrated, that cytokines as TNF-alpha are still there in the skin tissue.
So the most possible conclusion has to be: Chronic pain is a chronic low graded inflammation, like CRPS and NOT a psychological disease, caused by a former accident.
An inflammation is produced by the combined action of prostaglandins and cytokines.
If we are blocking the action of cytokines, we are blocking the inflammation too.
Infliximab is such a blocking agent. Two patients with CRPS had been cured by that.
The skin temperature is downgraded to normal as well.
In the hot spots of chronic pain the pain and the skin temperature has been downgraded by PTX. PTX and Infliximab have a -scientifically demonstrated- commonly effect: blocking of the inflammation activating cytokine: TNF-alpha. TNF-alpha actvivates the production of prostaglandins from cholesterol.
If the effect of PTX into painfully areas has been caused by the TNF-alpha blocking property the painful warm area in chronic pain must be caused by an chronic low profile inflammation! For this exists another scientifically argument.
In the end situation of CRPS the skin temperature is downgraded beneath the normal temperature. However pain exists as yet. One is seeing the same situation in case of cold chronic pain. In CRPS has been scientifically demonstrated, that cytokines as TNF-alpha are still there in the skin tissue.
So the most possible conclusion has to be: Chronic pain is a chronic low graded inflammation, like CRPS and NOT a psychological disease, caused by a former accident.
Next post. This thesis: phantasy or reality?
22-04-2018 Henk van der Veen.
27 April 2018 Posting 8.
Present: Fantasy or reality ?.
However there are many indications for the existence of the published model, those indications as such are not enough to prove the thesis. The proof will be accepted, when several scientists have confirmed, that cytokines as Interleukin 1, interleukin 6 and TNF-alpha are existing in areas of chronic pain. The same has been found in patients in the third phase of CRPS. The methods used to investigate this thesis are simply to realise. But nobody in the past had an idea to do so. In the case of CRPS F.J.P.M Huygen, professor in the treatment of pain at the Erasmus University , Rotterdam, the Netherlands, has done this in the years 2002-2004. For phase three of CRPS J Groeneweg has done this for his dissertation from 2008 till 2009.
This picture shows the way of research for the existence of cytokines:
 Photograph with permission of Prof.dr. F.J.P.M Huygen.
Photograph with permission of Prof.dr. F.J.P.M Huygen.
You can see the blisters, produced with a vacuum- pump. In this case ATMOS 350A. From the blisters an extraction has been made of 150 µ litre skin-tissue fluid. Huygen (“Mast cells are involved in inflammatory reactions during Complex Regional Pain Syndrome type 1. Immunology Letters 2004;91:147-54.”) has referred to the article of Michiels and Zijlstra: Michiels JJ,Zijlstra FJ. Prostaglandin cyclooxygenase products but not tromboxane A2 are involved in the pathogenesis of erythromyalgie in thrombocythaemia. Nediat Inflamm 1993; 2: 385-9. These method has been described in both publications. After 15 minutes at maximum the pressure of the vacuum-pump is down sized to 250 mm Hg, after 15 minutes again to 200 mmHg. This has been continued during 2-2.5 hours. The blisters after this process contained 150 µ litre skin-tissue fluid.
So the method isn’t quite difficult or costly. But world-wide one cannot find publications about that, applied to patients with chronic pain. Amazing when you realise that healthcare in the Netherlands spent 50 billion euro a year to the costs for chronic pain. The return of investment for such a research might be very profitable. In 1989 a study has been done by Van der Veen with Pentoxifylline as a rheological medicine used for chronic pain patients. The temperature in Cold spots increased and the temperature in Hot spots decreased. (P<0.001). The results have been verified in 2013 and the P value continued to be smaller than 0.001. From that moment Pentoxifylline has been successfully applied in a general medical practice as a treatment of chronic pain. The impact was explained in 1989 being an increase of oxygenation of the skin tissue. Unexplained was the downgrading in temperature in hot spot areas. Now we know, that Pentoxifylline (the used medicine) has a phosphodiesterase inhibiting effect and moreover an anti-inflammation effect by blocking of the pro-inflammatory cytokine TNF-alpha. The success-story of Pentoxifylline for treatment of chronic pain could be explained both in Cold and Hot areas by those characteristics. Concurrently the effect of Pentoxifylline points to the existence of inflammatory cytokines into the pain areas of the skin. There is an analogy with CRPS. Those cytokines are demonstrated in both the Hot and Cold phases of this syndrome after all. Moreover treatment with a TNF-alpha blocking agent have cured CRPS patients (Huygen and others). Pentoxifylline has TNF-alpha blocking properties too and the treatment costs are a hundred times lower than a modern biological ! So, for the man or woman, who dares, a scientifically scoop is waiting for you! The author can’t do it himself anymore. He is nearly 75 years and retired. From such a situation there aren’t practical opportunities. It is pity! But the grey cells are still working as you can see.
Henk van der Veen
Next post: executive summary.
Post 9. 24 May 2018
Recapitulation
Chronic pain deserves a new definition. Existing definition IASP (International Association for the Study of Pain): “Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage”. Pain is subjective. Every person is learning to use the idea “Pain”, based on his own experiences. The officially definition of the Dutch government for chronic pain is: “Pain had lost the primary function signalling dangerous situations and is going his own way”. But a new definition can be: “Chronic pain is an unpleasant sensory and emotional experience, staying more than 3 months and is based on the result of tissue trauma with an enduring inflammation in the tissue itself afterwards. It is possible to identify the resulting effects of the inflammation objectively and to treat them with medications. CRPS (Complex Regional Pain Syndrome) is an extraordinarily form of chronic pain, which differs only in the phase of the process.” Existing data about chronic pain:
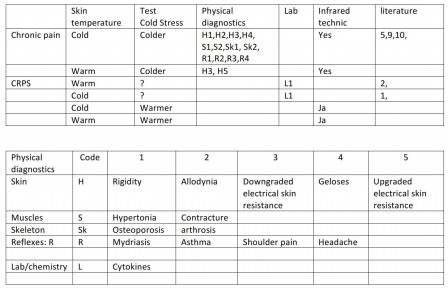
Tables: Measurable and objective controllable symptoms are definitely medical phenomena in case of chronic pain. They are not virtually symptoms really. There are publications about these symptoms in the skin, in muscles and skeleton. Both measurable in the classic way by medical doctors and physiotherapists, and with equipment for electrical resistance measurement and infrared thermography. Those symptoms have an interaction with each other at segmental level along reflex ways. There is quite a lot of literature about that. The codes in the upper table matches the codes of the lower table. Allodynie: IASP definition: “Allodynia is suggested for pain after stimulation which is not normally painful. Hyperesthesia includes both allodynia and hyperalgesia, but the more specific terms should be used wherever they are applicable.” It means, that stimulants, normally harmless, are causing pain in areas of chronic pain. Geloses are spindle and touchable hardenings in the connective tissue and the muscles. They are belonging to the segmental phenomena in chronic pain areas. Contractures are very intense convulsive movements of the muscles. Osteoporosis is a form of decalcification of the bones. Arthrosis is a form of irregular decalcification and ossification of the joints. Mydriasis is a pupillary reflex with widening. Asthma is a spastic constriction of the small airways with a severe obstruction of expiration. Cytokines are proteins with inflammable properties or just the opposite. They can be found in skin tissue liquids and it is possible to investigate them biochemically.
What does mean “Cold Stress” (11,12) ? “Cold Stress” is used for a test situation applied for Infrared Thermography. In the case of a pain-area in the arms: cooling down of the legs results normally in downgrading of the temperature of the legs and the arms. In reverse cooling down of the arms results in a lower temperature of the skin of the arms and the legs. It is a normal property of the autonomous nervous system. In some cases however the temperature in a pain area has been upgraded by using “Cold Stress”. That’s possible in both Cold and Warm areas. Cold stress upgrades the skin temperature in CRPS areas always. Upgrading of the temperature in cold areas is suspicious for an imminent CRPS. That’s in line with the former thoughts about the origin of CRPS: CRPS has its origin in an autonomous reflex-situation. The following elements are pleading for a relationship between Chronic pain and CRPS:
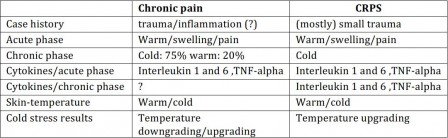
Chronic pain and CRPS are in many aspects look-alikes. Transitions from Chronic pain to CRPS are described being the same, but some differences exist. Most important is the fact, that CRPS upgrades in temperature in cooling experiments and chronic pain mostly downgrades. Besides there is none existing information about relationship between chronic pain and cytokines. In modern literature zero investigations are found with a causal relationship between chronic pain and former traumas or other tissue-damages.
Elements to be surprised about it. Nowhere in the world there has been found an university, which, interested in this questions, has published modern research about this theme. A theme with millions of patients and billions at costs. All the existing literature is very old.
Elements, partly conflicting with each other can be aggregated in a theoretical model yet. A model that scientifically can be verified. Tell me, why we have a theoretically Physics and an experimentally Physics and not an theoretically Medicine? Often the theory is leading the practice.
Using this model it is possible to explain, why chronic pain can be warm or cold, why the temperature of a chronic pain area under “Cold Stress” can rise or fall , why the temperature of CRPS under the same conditions always is rising. It can explain why chronic CRPS is cold and why the temperature with autonomic stimulation can rise again. It can explain too, why inflammation-active cytokines has been found in Cold CRPS. At last, but not at least, it can explain why CRPS is looking so “autonomic”. And all this is only based on research from 1977 of two excellent pharmacologists, which has been completely overlooked and already forgotten. Research with prostaglandins. That is making chronic pain so easy and at the same time so complicated. For understanding the phenomenon of chronic pain and CRPS one needs to have knowledge of four specialisms: the field of autonomic reflexes, the field of prostaglandins and cytokines, the field of infrared thermography and a piece of pharmacology. But in a segmented world of science there is no overlap. One cannot find a super-specialist with a helicopter view over all these collective areas. And without that it is very difficult for a scientifically approach of the phenomenon. Therefore is chronic pain spread out over all the practitioners and as you know: If chronic pain belongs to everyone, chronic pain belongs to no one.
Literature (Post 8 and post 9)
1) Groeneweg JG. Cold Case: Vascular dysregulation in the Complex Regional Pain Syndrome. Haveka BV.Alblasserdam. Dissertation. ISBN 978-90-9024512-6. 2009: 58. 2) Huygen FJPM. Neuroimmune Alterations in the Complex Regional Pain Syndrome. Proefschrift. 2004: 130-31 Internet: Available from http://www.erasmusmc.nl/pijn/research/promoties1/4142182/ 3) Huygen (“Mast cells are involved in inflammatory reactions during Complex Regional Pain Syndrome type 1. Immunology Letters 2004;91:147-54.”) verwees naar een eerder artikel van Michiels en Zijlstra: 4) Michiels JJ,Zijlstra FJ. Prostaglandin cyclooxygenase products but not tromboxane A2 are involved in the pathogenesis of erythromyalgie in thrombocythaemia. Nediat Inflamm 1993; 2: 385-9. 5) Veen PHE van der. Infrared thermography for pain influenced by a Xanthine derivative: An attempt to assess chronic pain objectively. Thermology Int. 2014. 24(2):39-48. 6) Pollice PF1, Rosier RN, Looney RJ, Puzas JE, Schwarz EM, O'Keefe RJ. Oral pentoxifylline inhibits release of tumor necrosis factor-alpha from human peripheral blood monocytes : a potential treatment for aseptic loosening of total joint components. J Bone Joint Surg Am. 2001 Jul;83-A(7):1057-61. 7) J Dubost, J & Soubrier, Martin & M Ristori, J & Beaujon, G & Oualid, T & L Bussière, J & Sauvezie, B. (1998). An open study of the anti-TNF alpha agent pentoxifylline in the treatment of rheumatoid arthritis. Revue du rhumatisme (English ed.). 64. 789-93. Available internet: https://www.researchgate.net/publication/13755195_An_open_study_of_the_anti-TNF_alpha_agent_pentoxifylline_in_the_treatment_of_rheumatoid_arthritis 8) Gail W. Sullivan,' Holliday T. Carper,' William J. Novick, jr. and Gerald L. Mandell'. Inhibition of the inflammatory action of interleukin-1 and tumor necrosis factor (alpha) on neutrophil function by pentoxifylline. Infection and Immunity, July 1988, p. 1722-1729 9) Baumann W. Ueber Thermometrische Untersuchungen im Zwlöffingerdarm und der Leber und der segmental zugeordneten Dermatomen. Munch Med Wschr. 1954;96: 605. 10) Veen PHE van der. Abdominal Wall Pain: Effects of Placebo Measured by Infrared Thermography. Thermology Int. 2014. 24(4) 157-165 11) Lahiri BB, Bagavathiappan S, Jayakumar T, Philip J.Medical applications of infrared thermography: A review. Infrared Physics & Technology 55 (2012) 221–235 12) Nahm, FS.Infrared Thermography in Pain Medicine. Korean J Pain 2013 July; Vol. 26, No. 3: 219-222. pISSN 2005-9159 eISSN 2093-0569 http://dx.doi.org/10.3344/kjp.2013.26.3.219
Henk van der Veen Next post: background of the thesis.
Post 10. 29 May 2018
Background thesis. part 1
From the preface has been demonstrated, that chronic pain detectable is in the SKIN. It has been originated as a result of bleeding, inflammation, bone fracture, operation or another kind of trauma in the skin directly. But not only directly. Also as a result of a combination of these factors in bones, joints, connective tissue, muscles and viscera. In this cases there has been an activation of visceral-cutaneous reflexes, ended in the skin. The visceral pain is nauseous and without the possibility of localisation. In combination with the skin component the pain is discernable in the same segment as the originating disease. The activity of this disease had been expanded to all the segment parts. That is giving possible problems with differential diagnostics.
An example:
An appendicitis normally is giving pain in the point of Mc Burney right down in the belly.
But the appendix has been located in the eleventh thoracic segment. As a result of this the eleventh intercostal muscle may start contracting too. In that case the pain starts in the upper part. In many cases this is leading to the misdiagnosis of a disease in the bladder.
Low back pain on the right side is another misleading symptom in the beginning of an appendicitis: Groups of fibres of the “Musculus Obliquus Abdominus” have been innervated from the same segment.
For a practioner the differential diagnosis is easy, based on physical signs.
After removal of an appendix a form of pain can left over. Mostly after a symptom less duration of three till six months. That kind of pain has been settled in the skin and in most cases it is chronic. After local anaesthesia in the skin the pain has been disappeared. The duration of this phenomenon can be twenty minutes to some days…. That is strange. The pharmacological time of working of the anaesthesia is about twenty minutes. What is happening in the organism after these twenty minutes ?. It is certainly NOT a jammed nerve. In that case the pain free duration is at maximum the duration of the effect of the anaesthesia. If the pain disappears for more than 24 hours there is another strange phenomenon: repetition of the anaesthetics leaves the pain for 48 hours, after another repetition about 96 hours and so on. Logarithms. Why ? These technique has been known as “Neuraltherapy” and has been used since 1925 mostly in Germany.
A third strange diagnostic finding is a result of infrared thermography (skin temperature measurement). The pain area described above is in thermographically measurement cold: the temperature is lower than the surrounding area. In the acute phase the area is warm. But when the infection has been gone. Why did the temperature not return to the normal state?
This example is presuming that “warm” is a property of an acute process and “cold” the property of an old process. Like a scar or a strangulated nerve. But in case of CRPS the end phase is Cold and yet there are inflammatory active cytokines. The same cytokines as in the warm acute phase and yet the skin is cold. It suggests there is still an inflammation. But inflammations have been considered to be warm, red and swollen. Why cold? And if there is an inflammation, is it possible that an inflammation exists in chronic pain areas too?
Is it possible to find a way to explain this? Yes there is such a way:
next post part 2
Henk van der veen
Post 11. 2 June 2018
Background thesis. part 2
Biochemically there is one substance, which has a role in pain, infection, inflammation, nerve activation, local anaesthesia, vasodilation and vasoconstriction together: the prostaglandins.
For inflammation they need to be bound on cytokines: inflammatory active proteins.
For vasoactive processes, they need to be bound on natural vasoactive proteins, like adrenalin and noradrenalin. Only in cooperation with proteins with a specific biologically action they can work.
In general prostaglandins do have two actions: they are sizing the magnitude of the effect of the effector and the art of the effect. They can design the art of the biochemically function of the active proteins. An example: they can change the activity of noradrenalin from vasoconstriction to vasodilation, just the opposite.
Normally in medical science one presumes, that a dose-effect curve for biologically action is a linear one. More prostaglandins the more effect. But research about prostaglandins already in 1977 showed another dose-effect curve: the "plateau phased and the “bell shaped” one. These curves are not a linear one.
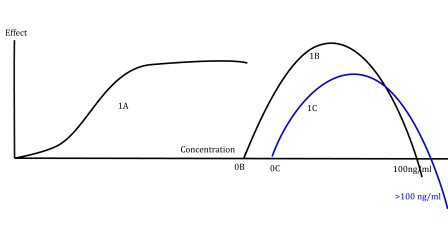 The concentration has been plotted logarithmically at the X-axis.
The top has been reached with a concentration of 1 nanogram/millilitre. Point “C” has been reached with a concentration of 100 nanogram/millilitre.
That’s very interesting. More than 1 ng/ml downgrades the prostaglandin effect.
More than 100 ng/ml changes the effect to the opposite.
So a vasoconstrictive prostaglandin in low doses (like PGE) is acting like a vasodilatative one (like PGF) in high doses. In inflammation with high concentrations PGE the skin tissue is reacting with vasodilation and exudation. The temperature of the skin tissue is then high. Returning to the healthy situation the concentration PGE is downgrading. As an example: the concentration PGE has been decreased so that the effect in excitation is on point “B”’ . Prostaglandin-“E” is acting vasoconstrictive. The temperature of the skin is much lower now than in the acute phase, but higher than with a concentration of 1 ng/ml. Yet the concentration in “B” is scarcely lower than 100ng/ml.
Above the concentration of 100 ng/ml PGE does enhancing the opposite PGF.
PGE has been reported as a pain generator too.
PGF has an opposite effect in relation to PGE. Above 100 ng/ml it is acting like PGE in low dose.
In a living organism the result of the both types together defines the final result.
As you can see the final result is dependent on the place of each prostaglandin effect upon the curve.
That place is dependent on the concentration of the prostaglandin.
The final result, applied to vasoactive situations, gives vasodilation with upgrading skin temperature or vasoconstriction with downgrading temperature. That can be measured with infrared thermography. But a good explanation of the results is not easy.
The concentration has been plotted logarithmically at the X-axis.
The top has been reached with a concentration of 1 nanogram/millilitre. Point “C” has been reached with a concentration of 100 nanogram/millilitre.
That’s very interesting. More than 1 ng/ml downgrades the prostaglandin effect.
More than 100 ng/ml changes the effect to the opposite.
So a vasoconstrictive prostaglandin in low doses (like PGE) is acting like a vasodilatative one (like PGF) in high doses. In inflammation with high concentrations PGE the skin tissue is reacting with vasodilation and exudation. The temperature of the skin tissue is then high. Returning to the healthy situation the concentration PGE is downgrading. As an example: the concentration PGE has been decreased so that the effect in excitation is on point “B”’ . Prostaglandin-“E” is acting vasoconstrictive. The temperature of the skin is much lower now than in the acute phase, but higher than with a concentration of 1 ng/ml. Yet the concentration in “B” is scarcely lower than 100ng/ml.
Above the concentration of 100 ng/ml PGE does enhancing the opposite PGF.
PGE has been reported as a pain generator too.
PGF has an opposite effect in relation to PGE. Above 100 ng/ml it is acting like PGE in low dose.
In a living organism the result of the both types together defines the final result.
As you can see the final result is dependent on the place of each prostaglandin effect upon the curve.
That place is dependent on the concentration of the prostaglandin.
The final result, applied to vasoactive situations, gives vasodilation with upgrading skin temperature or vasoconstriction with downgrading temperature. That can be measured with infrared thermography. But a good explanation of the results is not easy.
An example: After a fracture or an operation there is a release of a lot of cytokines, bound to prostaglandins (PGE and PGF). IF both the concentrations of PGE and PGF are smaller than 100 ng/ml and higher than 1 ng/ml the smallest concentration is essential for the resulting effect. Because of the smallest concentration is delivering the highest place on the curve.
In this example point “F” has a concentration smaller than 10 ng/ml and point “E” has a concentration higher than 10 ng/ml. The resulting effect is F-E and F>E. In this example there is a vasodilation, which can be measured by infrared thermography. In most physiologically healthy situations the concentrations prostaglandins are varying between picograms/ml and 1 nanogram/ml. In vigorously situations till 10 nanogram/ml. So there is a safety area of changing in concentrations. Estimated about a hundred times. This example shows a moderate inflammation, one can expect in case of a moderate appendicitis. Theoretically one can measure this with infrared thermography and on a biochemically way in skin tissue fluids. Not the prostaglandins itself, but still the cytokines onto the prostaglandins have been bound. Reversely, changing F and E, exists a vasoconstriction: a situation after recuperation in case of an infection. You see here a working modulating and regulating system of a living organism with a biochemically switch at point “C”. There is no other modulating and regulating system known or described in living organisms. And yes: Hormonal regulating is carried out by prostaglandins too. Applied to hormonal changes in the womanly cycle the model is published in 2015. Just as other biochemically active molecules hormones are bound with prostaglandins as a buddy. Without these buddies hormones does not have any activity. This model can explain the strange ambiguous findings mentioned above in this post. How ? That is, what you can read in the theoretical model itself. These posts are written only for step by step approaching the basics of this model.
In the next posts: the model itself and (more important) what can you do with that?
Henk van der veen
Post 12. 19 June 2018
Thesis. part 1
Introduction
The human body functions as a fully automated system. It has been told in previous posts.
Body temperature and biochemical processes are adjusted accurately without active humanly actions.
Therefore it is amazingly that the knowledge about that is missing to a high degree.
We know, that the autonomous nervous system plays an important role and we know that functioning of organs are modulated by hormones.
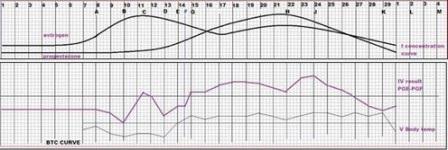 The upper curves are the concentration curves of estrogen and progestogen during the monthly female cycle. Smoothly and without any switching moments in the first two weeks. On the other hand the BBT (Basal Body Temperature) shows sharply peaks and dips.
The third curve is a calculated curve based on the switching properties of the prostaglandins , applied to the concentrations of the hormones. The lowest curve is an original BBT curve.
The original BBT curve and the reckoned one are very similar.
It has been known that prostaglandins modulate and regulate the action of hormones. The method of issue has not been documented yet. But the switching possibilities of them are looking very impressive.
All natures activities around the ovulation, reflected into the body temperature has been seen in the reckoned curve too.
The upper curves are the concentration curves of estrogen and progestogen during the monthly female cycle. Smoothly and without any switching moments in the first two weeks. On the other hand the BBT (Basal Body Temperature) shows sharply peaks and dips.
The third curve is a calculated curve based on the switching properties of the prostaglandins , applied to the concentrations of the hormones. The lowest curve is an original BBT curve.
The original BBT curve and the reckoned one are very similar.
It has been known that prostaglandins modulate and regulate the action of hormones. The method of issue has not been documented yet. But the switching possibilities of them are looking very impressive.
All natures activities around the ovulation, reflected into the body temperature has been seen in the reckoned curve too.
Switching functions
A switching function is an abrupt effect and not a fluently process. Everyone, who used a switch once in lifetime is knowing that.
An example: opening or closing a bridge is possible with the same switch. Two contrarily actions with the same button, activated in a split second.
Not known in the modern medicine, a similar biologically switch has been described in 1977 already.
Unfortunately that know-how had been too specialized for reaching the medical world. It is still waiting. The remarkable molecules having the property to produce two opposite effects have been described in the posts about prostaglandins.
But only one molecule with switching properties is not enough. In stable measure- and regulation systems there always exist two opposite action systems to balance each other.
Biological switches In the biologically world two types of opposite functioning prostaglandins are existing too, balancing each other. They had been researched and described as “vasodilatative” and “vasoconstrictive”, bound to a vasoconstrictive molecule. But as buddies to another pharmacologically active molecule they are doing much more. Bound to a hormonal system as the gynecologically combination estrogen-progestogen they have the ability to manage the body temperature. Result: the BBT.
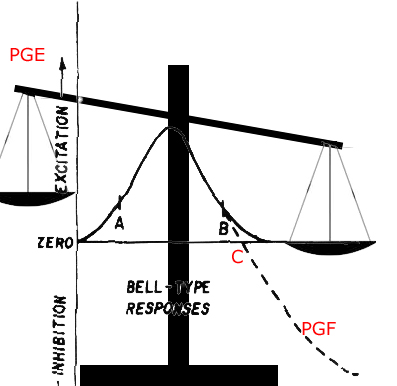
Theoretically the prostaglandins can be the link between the activity of the nervous system and the local biochemically processes. They can be the link between hormone concentrations and the effects attributed to hormones. Thereby they have the ability to switch. The curves, described by Horrobin and Manku are showing unmistakably that switch momentum: vasoconstriction to vasodilatation. Theoretically one molecule may be sufficient for changing the effect. As told earlier: two prostaglandins are known with switching properties: PGE and PGF. Only by one Hydrogen ion they are differing from each other. The biological system is able to change enzymatically PGE into PGF in a reversible way. At low physiologically concentration PGE is acting vasoconstrictive and PGF vasodilatative. At high concentration the effects are reversed. The effect of PGE minus the effect of PGF or vice-versa is presenting the resulting effect of both of them. Both prostaglandins have the same dose-effect curve. It means, that graphically the effects of both molecules are represented in a place on that curve.
Next post: Curves and PGE-PGF places on them.
Henk van der Veen
Post 13. 20 June 2018
""Thesis. part 2"
Curves and PGE-PGF places on them.
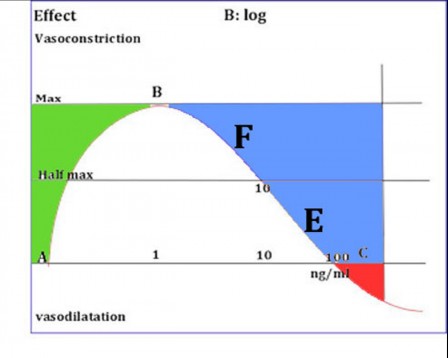
An example: Point “F” has been located on the descending leg of the curve with a prostaglandin PGF concentration between 1 and 10 nanogram/ml tissue fluid. (1 nanogram is one billionth of a gram.)(X-axis) The magnitude of the effect is between half max and max. (Y-axis). Point “E” has a concentration between 10 ng/ml and 100 ng/ml (X-axis). The magnitude of the effect is between half max and zero (Y-axis). In this example the effect of “F” corresponds to three times the effect of “E”. The concentration however is smaller than one fiftieth of the concentration of “E”. The effect of “F” is vasodilation. The effect of “E” is vasoconstriction. The net result in this example is a “moderate vasodilation”. However, the concentration of the vasoconstrictor is substantially more than that of the vasodilator. Like this a low concentration of an inhibiting molecule is blocking a (too) high concentration of an opposite working molecule. This is called a negative feed-back. The gynaecological example in post 12 shows physiological concentrations between 100 picogram/ml and 1000 picogram/ml (one picogram is one thousandth of a nanogram). In this example the green area. “Vasodilation” as a term of the activity of PGF can be changed in “lower sweating”, “more activity of the function of the gut”, “a lower airway resistance”, “better perfusion of the skin, connective tissue and muscles”. It is a situation in which inflammations can be developed. For instance: a beginning influenza (flu) starts with vasoconstriction and a cold. One is feeling cold too. The body temperature is lowering for a while. Suddenly that is changing in temperature upgrading and inflammation symptoms. In line with the model it means, that in a healthy situations both the concentration and effect of PGE and that of PFG has been located in the green area. In case of symptoms of disease point “B” of the curve is passed. Cold feelings and temperature downgrading can be started as a result of upgrading of the concentration of PGF. The PGF effect is downgrading then and the result from PGE and PGF is a PGE effect: vasoconstriction.
This example shows the situation in which the PGF-PGE balance is resulting in a PGE effect. It shows a “moderate vasoconstriction”. In this situation the term of activity of PGE :“Vasoconstriction” can be changed in :”sweating”, ”spastic guts”, “difficult defecation”, “spastic airways”, “viscous mucus”,” downgraded perfusion of the skin, connective tissue and muscles”, “Muscle spasms” and “lowering of the body temperature”. All these are symptoms, emerging in the pre-phase of a flu.
For the advanced scientists: all the described symptoms have been the result of a relationship between prostaglandins and Calcium ions, outside and inside a cell. If these ions from outside are passing the especially Calcium gates and not have been bound to especially peptides(Calmodulin) into the cell they are attached to small muscle fibers. The result is contraction. Just that is the property, which viruses need for cell injection and reduplication. Then the puzzle remains: Why and how the symptoms are starting with fever, vasodilation and so on? There is an answer: The dose-effect curve has the same fluent form for both antagonists. An abrupt moment only arises if one of them passes point “C” of the curve. If PGE passes point “C” the intrinsic property of vasoconstriction changes into vasodilation. The vasodilation property of PGF is upgraded by PGE. That is called a “positive feed-back”. The resulting effect is an inflammation. In all the modern literature PGE is called an inflammation active substance. But the reality is, that in modern experiments the test- dose always is higher than 100 ng/ml tissue fluid. And indeed: in that concentrations PGE has an inflammation effect, but not in physiologically circumstances.
Positive feed-back mechanisms are dangerous. The cross-current is missing and the process might to be unstoppable. That is the situation around CRPS. In the audio technique this phenomenon has been known as: acoustic feed-back. If a microphone is standing too nearby a speaker a shrill beep can ravage the ears! Also this phenomenon is a result of positive feed-back. The descending line of the curve is the most hazardous. Also in audio technique. In human bodies one can expect diseases, if the prostaglandin concentrations come along these line of the curve.
Next post (14): back to Chronic pain and CRPS Henk van der Veen
Post 14. 23 June 2018
Thesis. part 3
Thesis Back to chronic pain and CRPS
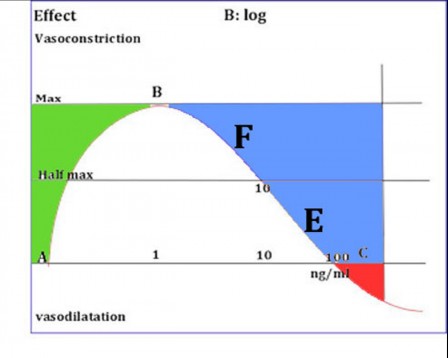
Both diseases are originated from damaged body tissue. Every kind of lesion gives rise to an inflammation process. Such a process is necessary for tissue repair. During the inflammation different kinds of peptides(cytokines)and prostaglandins are developed. These molecules are regulating the local recovery. The concentrations are easily upgrading to 10 ng/ml. Redness, swelling, pain and warmth are the results. The PGF effect controls the process. Therefore the concentration of PGE has to be higher than the concentration of PGF. Point “E” is closer to the switch point “C” of the curve than point “F”. A small upgrading of the concentration of PGE transfers point “E” to the red area beyond point “C”.
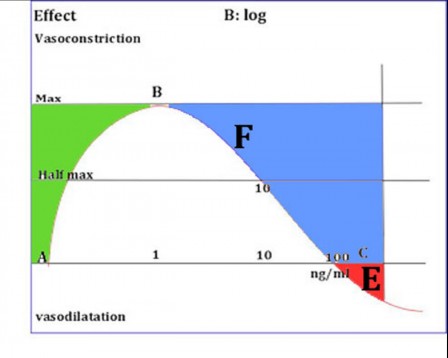
In this area the possibility to control the inflammation diminishes very dramatically. The properties of PGE are changed to vasodilation and inflammation. That is the medical situation seen in CRPS. With infrared thermography one sees an extended hot area in the swollen part of the extremity. The only opportunity to feed back for the organism is to upgrade the PGF concentration. The resulting inflammation effect is the downgrading of the temperature. Point “F” is moving to point “C”. At the phase of recovering of the disease the concentrations of inflammatory agents are decreasing. The concentration of PGE diminishes . The inflammation is decreasing and the temperature of the sick area downgrades. One can see that with the eyes and measure it with infrared thermography. But still the concentration of PGE is greater than the concentration PGF. (There is still vasodilation!). With further downgrading of the concentration of PGE the regulation changes again. The concentration of PGE is smaller than the concentration of PGF. It means that the PGE gets the control of the regulation. Vasoconstriction appears.
But the concentration PGF is still high. The concentration of the inflammatory active buddies too. But the area, measured with infrared thermography is cold now. There exists a cold inflammation, indeed. That is the situation, researched at the Erasmus University in Rotterdam (2008). In the tissue fluid of the “Cold CRPS patient” the same cytokines had been found as in the acute stage. That is in accordance with the model above.
In case of chronic pain there had been a lesion once. According to the situation of CRPS inflammatory active cytokines are produced in the tissue in the acute phase. Like CRPS in the recovery phase the painful area is , measured with infrared thermography, cold. Like CRPS, the concentration PGE has to be lower than the concentration PGF. Therefore the inflammatory active prostaglandin buddies have to be still present in the tissue . And so there must be an cold inflammation in areas with chronic pain. As described, a little lesion or operation has the possibility now to upgrade this situation to an active CRPS (again). So chronic pain and CRPS are not syndromes, but diseases. They differ from each other only by the phase in the same process.
Next post: diagnostics
Henk van der Veen
Post 15. 31 July 2018
Diagnostics in chronic pain and CRPS
Introduction
Infrared thermography.
Infrared thermography has been described extensively already in previous posts just as physically examination by doctors.
The leading principle in medical examination is physically at first. After that technically examination may be followed.
One single examination with infrared thermography is enough to direct the diagnosis, but it is often not enough for a properly diagnosis. It gives the possibility to find out the temperature of the pain area: warmer or colder than the referential area. The referential area is the zone around the pain area or the counter side in right or left sided pain. That temperature is important as well. Only two examination technics exist for determining the differences in skin temperature: technetium scanning and infrared thermography.
Technetium is a radio-actively drug with lightly radiation properties, produced in a few centres of the world. In the Netherlands it is produced in the reactor centre, located in Petten and only for medical use.
The drug is injected and accumulates in places with upgraded blood perfusion. Consequently the radiation accumulates too. With specially scanning equipment it is possible to measure that radiation. Reversely the radiation has been diminished in case of downgrading the blood perfusion.
In the eighties researchers had found a relationship between the radio-active radiation of technetium from painful skin areas and infrared thermography measurements. Infrared thermography is not damaging for environment and human beings and is also the preferred method for technical pain research. Unfortunately Infrared thermography is a rather unrecognized technique.
Warm pain Pain in a warm environment needs in his classical way inflammation with the symptoms: redness, and swelling . Chronic pain without a well-known cause shows those symptoms only in case of CRPS. 25% of chronic pain is warm without swelling and redness, demonstrated by thermographically research . CRPS has been investigated extensively, but warm chronic pain not. Still chronic warm pain can be the representative of an inflammation, even with the lack of swelling and redness. Also there is no research about the question if warm chronic pain can be the precursor of CRPS. And that is an important question.
Cold pain 70% of all chronic pain sites are cold In relation to their referential. It is not clear which processes are happening here in this tissue. It is never investigated. May be the results of CRPS research can help. CRPS is a furious inflammation, hardly to stop, but in the end phase of it there is not any visible inflammation anymore. Thermographically the tissue is cold, like the “normal” chronic pain.
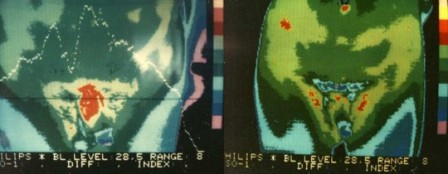
An acute CRPS with pain, swelling, redness.
Biochemical investigation of the skin tissue of cold CRPS is showing the same inflammatory cytokines like TNF-alpha as the active warm CRPS. So there must be an inflammation without redness and swelling. Cold inflammation. CRPS is an inflammation with a (small) trauma in his history. Also chronic pain has a trauma history, sometimes years ago. And like CRPS there had been existed a resulting inflammation like bleeding, fracture or haematoma. Sometimes there is a visible scar, but in most cases, there is nothing more to see, except by thermographically measurements. The invisible scar is cold. Fig.A Fig.B

The patient is lying in prone position from left to right. You see the buttocks. Black is cold. The black area on the lower panel (fig A) is a non-visible scar, a residue from an old trauma (hematoma) before treatment. Fig B is a picture after treatment. You see then a symmetrical image, like a cassata. That’s the ideal healthy situation.
So there is an analogue with CRPS. A cold area after a trauma with pain….. Logically like CRPS you can expect the area contains inflammatory cytokines as TNF-alpha too. Conclusion: a chronic low graded inflammation without warmth, redness and swelling is the most likely base of chronic pain without known aetiology. Thermographically the site is cold. Modern research is necessary to find out this hypothesis. But the consequences are immense. The technique is simple, relatively cheap, already done and described in case of CRPS. Who will be the first to do this in relation to Cold chronic pain?
As above described a single picture is giving only poor information.
Much more data are originated by a range of pictures in a test situation.
CRPS has been called “Autonomic Reflex dystrophy” In former times. That name is supposing the influence of the autonomic nervous system. One important test is using the activity of that system.
Normally (in healthy persons) the body temperature is lowering if the activity of the autonomous nervous system (sympathetic nervous system) has been stimulated. That is easy to realize. In some academic centres a “coolpack” is used. The temperature of a part of the body is cooled down under strictly regulated circumstances. But it possible on an easier way too. For a range of measurements at the upper extremities it is enough to cool down the feet’s and ankles in a little water basin with a temperature of 19 0C. Ten photographs within ten minutes. That’s all. Reversely for measurements at the legs one can do that with cooling down the hands and lower arms. The test is called: “Cold Stress Test”.
What can you see:
1. Cold areas become colder
2.Warm areas become colder
3. Cold areas become warmer
4.Warm areas become warmer.
In healthy persons temperature decrease is a normal reaction, but an increase is a pathologically reaction. What’s the consequence of this? At the same patient on the same moment it is possible to get both reactions: a decrease on the healthy side and an increase on the pain side. That is characteristic for (beginning) CRPS.
There are very clear similarities between chronic pain and CRPS, but they don’t form part of the regular medical science.
CRPS follows frequently small trauma’s. Chronic pain shows in his history frequent trauma’s , bleeding, hematoma’s or inflammation. In the final phase of CRPS scar tissue has been leaved.
Measuring with infrared equipment the area is COLD.
After recovery from a trauma, a bleeding, a hematoma or an inflammation sometimes a visible scar has been leaved, but looking with infrared light and special equipment one sees nearly always a scar: an area with decreased or increased temperature. Sometimes painful.
In only 5% of the cases painful areas are neutral in temperature. In 70% they are cold and in 25% warm. In the acute phase CRPS is always warm. Traumas, bleeding, fractures and inflammations are always warm in the acute phase too.
Fig C.
A patient with a painful area shortly after a bladder catheterization. (Left). The painful area is warm, but not swollen and no redness. The image reflect on the skin an internal trauma as a result of catheterization. The right image after three weeks: there is a lot of recovery. Neither visible scar nor visible signs.
These thermographically data are known at the neurological clinic of the University of Sao Paulo in Brazil. There exists a professorship for Infrared Thermography.
But else?
In the Netherlands there is not any knowledge about the origin of chronic pain, although there is extensive knowledge about that in old German literature. (Before 1945), but nobody is reading scientifically literature in German language after 1945. However all this literature is still showing much evidence about the origin of chronic pain and possibilities to treat it.
Modern papers from 2008 (Groeneweg), 2014 (Arendt-Nielsen), 2012,2013,2014,2015 (van der Veen) are pointing at a somatically and not a psychologically cause of chronic pain, like CRPS.
In the case of CRPS the tissue contains inflammatory active proteins: cytokines, like TNF-alpha, both in the acute phase and in the final phase. Chronic pain areas are containing the same cytokines in the inflammatory phase. About the final phase we did not know anything in the absence of research data, but it looks realistic that the same cytokines are causing the pain in the “chronic pain phase”.
Like CRPS!
But there are essentially remaining questions.
1.Inflammation has an unbreakable relation with warmth, redness and swelling too.
Why thermography is showing a cold inflammation without swelling and redness?
2.Sympathetic stimulation is contracting the vessels. (Skin)temperature is decreasing as a result.
Why autonomic stimulation has the property to raise the local temperature in some chronic pain areas?
3.There are too many similarities between CRPS and chronic pain.
Is there any relationship between them? Can it be?
4.In old papers the so called “CRPS” has been described as “Autonomic reflex dystrophy”.
That terminology has been leaved in favor of “CRPS”.
Is it yet possible, that autonomic (sympathetic) stimulation might provoke a process as “CRPS”?
The answer is: Yes, all this is possible and reasonable and verifiable with infrared thermography, followed by biochemically testing of tissue fluid from the measured places.
Why it has not been done this? I don’t know. Someone must be the first? Maybe someone anywhere on the world in the future. You can hope so.
In post 16 the tests are described by means of a model of chronic pain, based on the origin of chronic pain as a chronic inflammation. In post 17 specific therapeutic possibilities are described, based on this model.
Henk van der Veen
Post 16. 24 Augustus 2018
Diagnostics in a new Model of Pain and CRPS
Diagnostic findings with infrared thermography, in relation to a new model of chronic pain.
Normally it is wise to explain a model before presenting it. However I have made the choice to do that afterwards, because a model is an abstraction too. It is easier to concretise by an explanation after the presentation.
Summary of the previous posts.
First:
{From the skin vasodilation can be measured by temperature increase and vasoconstriction by temperature decrease. The model has as fundamental idea that the skin is responsible for generating the experience of chronic pain. Chronic pain is disappearing temporarily (sometimes longer) after local anaesthesia of the area of pain in the skin. Local anaesthetics are blocking prostaglandins and prostaglandins have vasoactive effects. Those effects are measurable by infrared thermography.}
Second
Different findings have been showed, which are looking to conflict with each other.
Some of them are appearing to interfere with a scientifically explanation. That is the same contradiction scientists have been found in a new group of biochemically active compounds in the sixties and seventies of the past century. The group of prostaglandins. Thousands of scientifically papers have appeared, but the results are very contradictory. But finally everybody have found each other in some crucially conclusions: Prostaglandins alone do not have any biologically effects! Only functioning as a buddy together with another biologically active compound they modulate and regulate that function. They have a role in muscle activity, blood vessel perfusion, pain, inflammation, activity of nerve cells and nerve fibres and hormonal activity.
One can find them anywhere in the body. They are originated and destructed locally. Their biological half live is very short. If they passed into the blood circulation they have been disappeared within one passage. Because they don’t have a biologically effect alone, but only modulate and regulate effects of other biologically active compounds, they are called locally hormones.
In relation with the phenomenon of chronic pain their effects in originating pain, inflammations and activating or inhibition of the activity of the nervous system have an extraordinarily significance.
Nothing produces nothing. Also pain doesn’t appear from nothing. Pain is an actually signal. There is something happening! For chronic pain especially inflammation is an important element.
Every trauma of the human tissue is originating an inflammation. Mostly temporarily. Inflammation is a normal and essential side-effect in wound-healing. Prostaglandins are the leading factors for a normal course of that process.
A memory of pain seems not to exist. It is difficult to quantify formerly pain, if the pain has been leaved. That is pointing to an actual temporary pain sensation.
In 1977 some papers are published about the activity of a range of prostaglandins, which could be produced synthetically. The results of in vitro research with muscle preparations. Only in such a situation is reliable research with low doses of prostaglandins possible. For that it is necessary to shut down the whole physiologically prostaglandin synthesis in the preparation. Therefore is used indomethacin as blocking agent mostly. Indomethacin is a drug, which is used in living humans for inhibition of inflammation or pain too. It is clear, that a complete shut-down of the body’s own prostaglandin synthesis is not possible in living humans. The human is dead then.
So there is always interfering with physiologically produced prostaglandins. The physiologically concentrations are lying between femtograms and picograms per millilitre body tissue fluid. (one millionth of a billionth per millilitre till one millionth of a millionth per millilitre).
And just that can explain the differences between the found results.
It is a strange matter the way of thinking about a linear dose-effect relationship in the area of pharmacology. It means that the effect has been supposed to be doubled, when the concentration has been doubled etcetera, etcetera.
 However the reality for many biochemically active compounds is not a straight line, but a bell shaped curve in most situations.
However the reality for many biochemically active compounds is not a straight line, but a bell shaped curve in most situations.
 The difference is clear. Above a certainly concentration (“B”) the effect do not increase anymore, but decreases. Moreover the effect changes reversely above a higher concentration.
In this example the effect changes from vasoconstriction into vasodilation.
Horrobin and Manku had demonstrated this definitely in 1977 already.
The difference is clear. Above a certainly concentration (“B”) the effect do not increase anymore, but decreases. Moreover the effect changes reversely above a higher concentration.
In this example the effect changes from vasoconstriction into vasodilation.
Horrobin and Manku had demonstrated this definitely in 1977 already.
The modification of their results has been demonstrated in this Blog earlier.
 The X-axis represents the concentration of prostaglandins in a logarithmically scale. A: zero and C: 100 ng/ml. The Y-axis shows the effect: vasoconstriction or vasodilation. The concentration level of 100 ng/nl forms the switch.
Some different types of prostaglandins are known with the same parabolic curve. Two types are important in this model : Prostaglandin E (PGE) and prostaglandin F (PGF). According the results of Horrobin and Manku PGE is acting like a vasoconstrictor in low dose and PGF as a vasodilator.
The own physiologically prostaglandin production in their preparation had be set on zero first.
However it is remarkable that most researchers are reporting a stimulating effect on inflammation with vasodilation of PGE. The contrary is reported about PGF!
Reviewing the papers with these results shows that most of these results have been reached with existing levels of physiological prostaglandins as a base. The conclusion must be that in most cases not low (physiologically) levels have been measured, but levels above 100 ng/ml, therefore after the switch. In the model we shall see the significance of that in different options. We can measuring that with infrared thermography in specific physiologically test situations.
Because PGE and PGF are counteracting each other a resulting action exists. (PGE-PGF or PGF-PGE).
In this model is showed the action of PGE as “E” and the action of PGF as “F”.
In formerly versions of the model the Y-axis seems to represent vasoconstriction. That’s confusing with showing the levels of effect both of PGF as PGE. They are counteracting.
It is better to show the Y-axis as a level of action. If E>F the result is vasoconstriction. If F>E the result is vasodilation.
The X-axis represents the concentration of prostaglandins in a logarithmically scale. A: zero and C: 100 ng/ml. The Y-axis shows the effect: vasoconstriction or vasodilation. The concentration level of 100 ng/nl forms the switch.
Some different types of prostaglandins are known with the same parabolic curve. Two types are important in this model : Prostaglandin E (PGE) and prostaglandin F (PGF). According the results of Horrobin and Manku PGE is acting like a vasoconstrictor in low dose and PGF as a vasodilator.
The own physiologically prostaglandin production in their preparation had be set on zero first.
However it is remarkable that most researchers are reporting a stimulating effect on inflammation with vasodilation of PGE. The contrary is reported about PGF!
Reviewing the papers with these results shows that most of these results have been reached with existing levels of physiological prostaglandins as a base. The conclusion must be that in most cases not low (physiologically) levels have been measured, but levels above 100 ng/ml, therefore after the switch. In the model we shall see the significance of that in different options. We can measuring that with infrared thermography in specific physiologically test situations.
Because PGE and PGF are counteracting each other a resulting action exists. (PGE-PGF or PGF-PGE).
In this model is showed the action of PGE as “E” and the action of PGF as “F”.
In formerly versions of the model the Y-axis seems to represent vasoconstriction. That’s confusing with showing the levels of effect both of PGF as PGE. They are counteracting.
It is better to show the Y-axis as a level of action. If E>F the result is vasoconstriction. If F>E the result is vasodilation.
 In a healthy physiologically situation the vasoactive properties of the prostaglandins are measurable with infrared thermography. That is useful for measurements of physically exercise par example, but infrared thermography is useful for testing of diseases or prevention too. Especially in case of chronic pain and CRPS. Then it is the first choice.
There is one method for producing prostaglandins in the human body without tissue damaging. It is called “Cold Stress”. A part of the body is cooled down by a cooling body pack. During the cooling down procedure the orthosympathetic part of the autonomous nervous system is stimulated. By the resulting prostaglandin “E” (PGE) is the normal reaction in a healthy person: vasoconstriction. The skin temperature decreases, not only within the body pack, but over the whole body surface. That is the result of an autonomous reflex. There are more easier and cheaper ways to do this: Within the thermographically departments of medicine Cold Stress is generated by cooling down feet or arms into a footwell with water of 19 degrees Celsius during ten minutes. That is sufficient. In generally it is possible to make ten measurements: every minute one. It delivers a lot of information. Cheap, safely and harmless.
With cold stress there are six possibilities to study:
In a healthy physiologically situation the vasoactive properties of the prostaglandins are measurable with infrared thermography. That is useful for measurements of physically exercise par example, but infrared thermography is useful for testing of diseases or prevention too. Especially in case of chronic pain and CRPS. Then it is the first choice.
There is one method for producing prostaglandins in the human body without tissue damaging. It is called “Cold Stress”. A part of the body is cooled down by a cooling body pack. During the cooling down procedure the orthosympathetic part of the autonomous nervous system is stimulated. By the resulting prostaglandin “E” (PGE) is the normal reaction in a healthy person: vasoconstriction. The skin temperature decreases, not only within the body pack, but over the whole body surface. That is the result of an autonomous reflex. There are more easier and cheaper ways to do this: Within the thermographically departments of medicine Cold Stress is generated by cooling down feet or arms into a footwell with water of 19 degrees Celsius during ten minutes. That is sufficient. In generally it is possible to make ten measurements: every minute one. It delivers a lot of information. Cheap, safely and harmless.
With cold stress there are six possibilities to study:
1. Cold skin areas are colder 2. Warm skin areas are colder 3. Cold skin areas are warmer 4. Warm areas are warmer 5. Threatening CRPS 6. Beginning CRPS
Active CRPS doesn’t need testing. Diagnosis by questionnaires and a “hot picture” is sufficient. Cold stress will damage the tissue by activating the inflammation! Temperature decrease during the test is a normal physiologically reaction, but an increase is always pathological. The old term for CRPS is “Autonomic reflex dystrophy”. However temperature increase by Cold Stress is normally not comprehendible. May be that is a reason to change the term of “Autonomic reflex dystrophy” into “CRPS”. That discrepancy forms the base of the model: Chronic pain and CRPS are NOT different diseases, but only different PHASES from the same disease. You can see it in the figure above.
Back to the possibilities.
Cold skin areas are colder
 In this model a cold painful skin area means a resulting PGE effect. PGE-PGF>0
The effect has been plotted on the Y-axis. So point E must be higher on the Y-axis than point F.
In this model a cold painful skin area means a resulting PGE effect. PGE-PGF>0
The effect has been plotted on the Y-axis. So point E must be higher on the Y-axis than point F.
Point E has two theoretically places: High on the ascending leg of the curve or high on the descending leg. (E or EX). EX cannot be the place, because by cold stress the prostaglandin concentration increases and therefore EX falls to the X-axis. The difference between EX and F becomes smaller and the temperature increases. But we measured a temperature decrease.
Therefore is E the right place. It has to be between concentrations of 500 and 1000 picogram (1000 picogram=1 nanogram) per millilitre. F has to be between 10 and 100 nanogram per millilitre. With increasing prostaglandin (PGE) concentration there is a shift toward point B. The difference between E and F increases and the temperature decreases. And just that we are measuring.
Warm skin areas are colder
That’s a normal situation in the recovery stage of an inflammation.

In fact this is a physiologically situation. It represents an compensating balance between PGE and PGF with the possibility to give negative feedback, a normal condition for every stable measuring and regulation system. F has to be high on the curve, above the level of E. There has to be a positive result between F and E. (F-E>0). The physiological result is vasodilation and a warm skin area. Point E cannot be on the descending leg of the curve, because the risk to provoke a CRPS. That would be a dangerous situation instead of a physiologically process. (see: warm areas are warmer).
Cold skin areas are warmer.
 The first image in the measuring process is showing a cold skin area. Therefore point E has to be higher on the curve than point F. Point E cannot be on the ascending leg: with cold stress the concentration increases and the vasoconstriction too. The only possible place is high on the descending leg. (Point EX). With increasing concentration PGE the effect decreases and vasoconstriction is diminishing then. The result is vasodilation and a skin temperature, which is increasing.
By some researchers this situation is called CRPS too, but probably the CRPS questionnaires are still negative. In fact it is a risky phase in originating CRPS. These patients should not to be operated trying to cure them from their pain. Active CRPS can be expected.
Another group of patients should not be operated due to their pain too. The CRPS risk is even more higher.
The first image in the measuring process is showing a cold skin area. Therefore point E has to be higher on the curve than point F. Point E cannot be on the ascending leg: with cold stress the concentration increases and the vasoconstriction too. The only possible place is high on the descending leg. (Point EX). With increasing concentration PGE the effect decreases and vasoconstriction is diminishing then. The result is vasodilation and a skin temperature, which is increasing.
By some researchers this situation is called CRPS too, but probably the CRPS questionnaires are still negative. In fact it is a risky phase in originating CRPS. These patients should not to be operated trying to cure them from their pain. Active CRPS can be expected.
Another group of patients should not be operated due to their pain too. The CRPS risk is even more higher.
Warm pain areas are warmer
Point E is located with a high concentration PGE nearby point C.
 The area is warm. Point F has to be located high on the descending leg of the curve. Vasodilation predominates. Theoretically should it be possible that Point F and point E are to be located on the ascending leg of the curve, but that is a physiologically situation. The concentrations of PGF and PGE are too low for producing pain then. Only F can be located high on the ascending leg, but it is unlikely that such a low concentration of PGF can be combined with a high concentration PGE.
A physiological situation at one hand and a pathological at the other together…. That is not a logically combination.
Anyway the result is vasodilation and the temperature of the pain zone increases.
There is an high risk for CRPS:
The increasing concentration PGE by cold stress can pass Point C (100ng/ml) and then PGE becomes vasodilatative and inflammatory properties enhanced by the intrinsic properties of PGF.
There is a positive feedback and CRPS is starting.
Therefore this situation is classified by some researchers as CRPS too, but there are possibilities for negative feedback still. Strictly there is not a matter of CRPS yet.
Remarkably is the fact, that CRPS in old literature is called “Autonomic reflex dystrophy”. That term has been lost by new immunologically insights about the origin of CRPS. However this old aetiology is returning with this model.
A situation in which the concentrations of PGF and PGE both are laying between ten and hundred ng/ml can be called as threatening CRPS.
The area is warm. Point F has to be located high on the descending leg of the curve. Vasodilation predominates. Theoretically should it be possible that Point F and point E are to be located on the ascending leg of the curve, but that is a physiologically situation. The concentrations of PGF and PGE are too low for producing pain then. Only F can be located high on the ascending leg, but it is unlikely that such a low concentration of PGF can be combined with a high concentration PGE.
A physiological situation at one hand and a pathological at the other together…. That is not a logically combination.
Anyway the result is vasodilation and the temperature of the pain zone increases.
There is an high risk for CRPS:
The increasing concentration PGE by cold stress can pass Point C (100ng/ml) and then PGE becomes vasodilatative and inflammatory properties enhanced by the intrinsic properties of PGF.
There is a positive feedback and CRPS is starting.
Therefore this situation is classified by some researchers as CRPS too, but there are possibilities for negative feedback still. Strictly there is not a matter of CRPS yet.
Remarkably is the fact, that CRPS in old literature is called “Autonomic reflex dystrophy”. That term has been lost by new immunologically insights about the origin of CRPS. However this old aetiology is returning with this model.
A situation in which the concentrations of PGF and PGE both are laying between ten and hundred ng/ml can be called as threatening CRPS.
Threatening CRPS
There are two possibilities. One from a cold starting position and one from a warm.

This example is a cold one. The resultant effect is a vasoconstriction. If the positions of F and E have been interchanged the resultant effect is a vasodilation. This position is very risky. A little event can cause a vasoconstriction with positive feedback, a situation, as one can see in case of the seldom occurring disease of Rye, or a vasodilation with positive feedback like CRPS. Autonomic stimulation with cold stress, producing PGE, gives rise to a CRPS. In case of a cold starting position questionnaires will be negative. In case of a warm starting position some questionnaires will be positive. By some researchers this position will be called as CRPS too, but strictly it is not a CRPS. The feedback possibilities are still negative.
When the PGE concentration passes 100 ng/ml there is definitely an active CRPS.
Active CRPS
 F is producing a vasodilation. E produces now inflammation and vasodilation. There exists an active positive feedback. Every counteraction is intensifying the inflammation process. As prof Huygen wrote in his dissertation already: It is nearly impossible to set off the inflammation process. And it is. Nearly. In physics such situations are well-known. There exist two types of interventions. More about that in the post about therapeutic possibilities. They are!
F is producing a vasodilation. E produces now inflammation and vasodilation. There exists an active positive feedback. Every counteraction is intensifying the inflammation process. As prof Huygen wrote in his dissertation already: It is nearly impossible to set off the inflammation process. And it is. Nearly. In physics such situations are well-known. There exist two types of interventions. More about that in the post about therapeutic possibilities. They are!
The actual value of this model
This model is not a pure academic one. In my opinion medical research must have an intention of practical application. Prevention and curing of diseases, that are the essentials of medicine. And a model ought to serve this principle too. So there are practically aspects. First, because it clarifies that chronic pain and CRPs are not separate conditions, but phases of the same disease. Indeed disease and not a psychological circumstance or some kind of syndrome. It shows, that chronic pain and CRPS could be consequences of preceding accidents with additional inflammations. The optical characteristics of inflammation are disappearing, but in many cases prostaglandins and cytokines with not physiologically concentrations are remaining with vasoconstriction and nerve stimulation as a result. So a fundamentally locally biochemical process can have an extensive continuation in the central nervous system, with a virtually realisation of a copy of the original process in that nervous system, proceeded up to the pain centres in the brains. Herefore others found arguments in the last years. The fundamentally local processes are appearing in the skin, functioning as an interactive human monitor, interacting actively by reflexes with visceral, skeletal, muscular and connective tissue, parts of the same segment. In generally they are hidden for the naked eye, but not for infrared equipment. So it had been possible to overlook these processes during more than hundred years and still! In the second place shows the model the different representations of chronic pain as precursors of CRPS. Representations, which are simply measurable and testable. As a result of that possibilities are existing to avoid CRPS by small operations. In the third place the model facilitates aimed and rational therapeutic actions.
I am aware of the weight of this claim, but I used the techniques during 40 years without knowing why. And it had worked and more: those techniques are obvious testable. But as in each science: It takes more than one swallow to make a summer. Let them come. Structured repetition is needed. And for that a model is serving too.
Post 17. 09 September 2018
Therapeutics in a new Model of Pain and CRPS
Post 17
The final post about the new model of chronic pain.
Existing and new therapeutic possibilities according to the new model. Both for chronic pain and CRPS there are theoretically possibilities based on rationally medical insights. Some of them are used in practice already. However the tradition of trial and error is still applied in most cases, not bothered by scientifically arguments. Even if that is not necessary.
Introduction
First of all chronic pain will be discussed, simply because the author has been started with that 45 years ago and because chronic pain in the new model is considered as the possible precursor of active CRPS. Handling of chronic pain therefore means a prophylactic approach of CRPS at the same time. The fundamental idea of treatment in the context of the new model is the argumentation, that a bleeding, fracture or operation always is followed by an inflammatory process. Required for a normal recovery process. However not every patient is recovering completely. It is a complex event in which prostaglandins are playing an essentially role. That are very unstable molecules, much more than the peptide molecules with which they have been combined. (And have to combine vice versa).
The peptides, called cytokines, exist in two kinds: activating or inhibiting inflammatory processes. There is a relationship between prostaglandins and pain. Pain is an accompanying phenomenon in case of tissue damage. The signal of it is actual and normally temporary if the tissue has been repaired. However people, who don’t have pain sensation at all, have a fast degeneration of the joints. The mechanism for that is unclear and it doesn’t mean that pain stimulates tissue repair. It is more likely, that the same mechanisms in which pain has been involved are influencing tissue repair too.
So far this shortly summary , needed for understanding the art of pain therapeutics.
Pharmacology
Prostaglandins
Pain has been treated with medicines since the beginning of the 20th century already. With anaesthetics like alcohol and opium probably centuries earlier. A drug like aspirin has been developed because willow bast had been used as a local treatment of pain and inflammation of the skin. The biologically active principle was salicylic acid. But that turned out to be too harming for the stomach wall. Coupled to acetic acid the drug had been much safer. The aspirin had been born.
Another painkiller had been found as a result of aniline research. A derivative, named as Novaminsulfon showed itself to have painkilling properties. Both aspirin and novaminsulfon are used to date as the most important pain inhibiting pharmaceuticals in the world.
Today we know, they are working by inhibiting the prostaglandin synthesis from cholesterol. Pain is inhibited by decrease of the prostaglandin concentration.
Besides the peripherally prostaglandin synthesis from cholesterol there is another and also important way to produce the prostaglandins. Release from the cell wall itself. This way of production is regulated by adrenocortical steroid hormones like prednisone.
But not only by inhibition of the prostaglandin concentration pain can be diminished. Also by blocking of their activity. Drugs like cocaine, morphine and other such have such properties.
They have the capacity to penetrate the blood-brain barrier and reach the central nervous system.
Therefore they are called central analgesics in contrast to the prostaglandin synthesis inhibitors, which are called peripheral analgesics.
A special group has cocaine as starting point. In the French-German war at the end of the 19th century there was an important need for local anaesthetics. Besides the local anaesthetic action on the eye, cocaine showed a proved local effect after injection. But the side effects had been unwanted. In the first decades of the 20th century scientifically research had been resulted in a new local anaesthetic named procaine. At today procaine is used in a special branch of complementary medicine, developed in Germany and known as Neural therapy. Succeeding local anaesthetics with lidocaine as an important representative are used in the medical practice today.
For chronic pain treatment ” Neural therapy” is very effective. The local anaesthetics have been proven prostaglandin agonists and antagonists.
Nowadays electronic equipment and surgical methods have been used to diminish pain too, but these techniques are out of the scope of this pain model. That is a biochemically model and the possibilities for treatment will be concerned within this model. So pharmacologically.
Besides the drugs acting on the behaviour of prostaglandins there exist another element for influencing pain, not yet implemented in the medical practice: the buddy-coupling element of prostaglandins to cytokines.
Cytokines
Medically intention is pointed to the prostaglandins or the cytokines, dependent of the interest in pain or inflammation. But in reality prostaglandins and cytokines are working together in pain and inflammation. So you can expect that blocking of cytokines is resulting in decreasing of pain too. In the eighties of the 20th century prostaglandins had been a well-known research item, but cytokines not or scarcely. Still then had been started a research-project with a cytokine-blocker in case of chronic pain, without the knowledge about that pharmacologically aspect. Accidentally. The idea behind the research project had been evolved from the findings, that chronic pain is generated in the SKIN and the phenomenon of vasoconstriction in 75% of the areas with chronic pain. We expected, that vasoconstriction and the resulting lack of oxygenation might be the spring of pain generation. Only in 1986 we had to our disposal accurately measurement equipment and a new pharmaceutical for better perfusion of narrowed vessels. And indeed, it had been worked. Pain decreased and the skin had been perfused left and right sided symmetrically. Only recently in the 21th century the underlying biochemical details has been known. The drug : pentoxifylline (PTX) sold as Trental® is acting like a phosphodiesterase inhibitor and is blocking some specific cytokines. Result: vasodilation and blocking of inflammation. These cytokines are produced in high quantity in case of traumas, inflammations, fractures and (orthopaedic) operations. In most cases they are disappearing when recovery has been finished. That is normal, because they have a function in tissue repairing. But it seems, that the recovery in some people has not been completely. The activity of Trental® is looking suspicious for a cold chronic form of inflammation in the scar area, even if the naked eye cannot see a scar. But infrared thermography is able to measure it. Due to the combined properties of pentoxifylline it looks as the first choice pharmaceutical in case of chronic pain. More suitable than the blocking agents of the prostaglandin synthesis only , not addictive or habit-forming like oxycodone and much more cheaper than modern biologicals as infliximab. It is amazing that it has not been used yet.
CRPS
It is much easier to see CRPS as a disease than to do the same with chronic pain. Chronic pain has to be rid of his psychologically phantom first. Besides CRPS has been investigated thoroughly already.
Therefore it is amazing, that the results of all these investigations did not have resulted into practically treatment. In the case of CRPS many cytokines had been produced and analysed. Cytokines as described above. Together with their prostaglandin buddies they are causing a severe inflammation, without hardly negative feedback possibilities. The huge amount of prostaglandins are locally produced from cholesterol and cell wall elements. Neither the cell wall prostaglandins, nor the cytokines are blocked by the usually techniques. Still there have to be possibilities to handle CRPS with pharmaceuticals, blocking the cytokines. One patient has been cured in Rotterdam with a modern biological (infliximab) and described as a case report. The extremely high costs of that biological is discouraging further investigation impossible. But as described above there exists another old and cheap pharmacological, which has the possibilities to block the same cytokines as infliximab. Contrary to infliximab (€ 19000 a year) Trental® costs about € 250 a year.
Today it is used for blocking TNF-alfa only in experiments with animals.
But Trental® is a normally registered pharmaceutical for better perfusion of the vessels.
The Erasmus university is possessing a fully followed and described case of CRPS, treated with Infliximab. I have a fully followed and described case of CRPS, treated with Trental®. Both patients are cured. So where is the blockade for further investigation?
Prevention
Prevention of CRPS is an important matter. Even more it is possible on an easy way. In the model chronic pain can result in CRPS with small traumas or by stimulation of the autonomic nervous system. In case of trauma it is looking logically: much cytokines have been produced in the body tissue. However, what is the role of the central nervous system? That is to investigate with testing. With cold stress alone the infrared measured values in CRPS have been worsened. After taking a test dose PTX (Trental®) the infrared values with cold stress are nearly normal. That is suggesting a stimulating effect of the autonomous nervous system on activating CRPS by activating the cytokines. As a consequence of that patients with a CRPS risk, namely those pain patients with a temperature increase after cold stress, can be expected to have a profit in using Trental® in risky situations. Risky situations are elite sport and planned non-deferrable operations in a pain area. That is a rationally directed therapy as a prevention of a worsening case. It is possible. The possibilities exist more than thirty years already, but are not used yet.
It is pity.
Henk van der Veen.
Published on 01/03/2018 by Henk